Adaptation
Staph infections have plagued people for centuries. It was officially named by doctors in the 1880's when they realized that this type of infection caused most of the infections that occurred after surgery. In the 1940's, penicillin was discovered by accident by Alexander Fleming in 1928 (Harvard Women's Health, 2008).
 When doctors figured out
that they could give penicillin to their patients to help them
kill the Staph infection, most Staph infections were no longer
deadly. Until this point, these infections had been the death of
their victims, but now, once patients were given penicillin,
they were generally saved. To learn more about penicillin
go to
Penicillium chrysogenum.
When doctors figured out
that they could give penicillin to their patients to help them
kill the Staph infection, most Staph infections were no longer
deadly. Until this point, these infections had been the death of
their victims, but now, once patients were given penicillin,
they were generally saved. To learn more about penicillin
go to
Penicillium chrysogenum.
This was working great until there were some resistant Staphylococcus aureus. This resistant strain contained an enzyme called penicillinase which broke down the penicillin and protected the bacteria against this drug. Since natural selection favors alleles with this resistance, penicillin was no longer working for many of the infections that it been able to cure before. (www.dh.gov.uk)
Bacteria can easily adapt to its environment. It does this by having a mutation which increases the likelihood that it will be able to live even in the presence of antibiotics. Some mutations are enzymes that deactivate the enzyme, others eliminate the site where antibiotics would enter the cell, and others allow the bacteria to pump out the antibiotic before it can do any damage. (Harvard Women's Health, 2008)
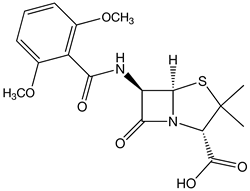 In 1959, 90-95% of Staphylococcus aureus infections
were resistant to penicillin (www.dh.gov.uk). Obviously, penicillin could
not be used anymore because it was no longer effective. A
new drug had to be found that could be used to treat these
infections that wouldn't be broken down by the enzyme penicillinase. This new drug was methicillin.
In 1959, 90-95% of Staphylococcus aureus infections
were resistant to penicillin (www.dh.gov.uk). Obviously, penicillin could
not be used anymore because it was no longer effective. A
new drug had to be found that could be used to treat these
infections that wouldn't be broken down by the enzyme penicillinase. This new drug was methicillin.
Within one year of using this new drug, the first case of MRSA was reported. Staphylococcus aureus become resistant to methicillin also because of penicillin-binding protein that is coded by the methicillin resistant gene also known as meCA. It has also been shown that MRSA is able to evade attacks by antimocrobial peptides (AMPs) and other parts of the hosts innate defense (Li, 2007). MRSA remained relatively quiet throughout the 60's and 70's, but in the 90's, it became more and more common. Today, it is estimated by the Kaiser foundation that 1.2 million hospital patients are infected by MRSA each and every year (www.medicine.net). That number is staggering considering that this doesn't even include the number of people who are infected outside of hospitals each year.
seubert.heid@students.uwlax.edu