Pathology of Clostridium difficile
 How does Clostridium difficile enter
the body?
How does Clostridium difficile enter
the body?
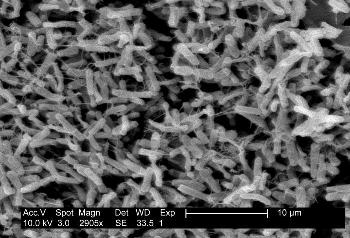
C. difficile enters a
person’s body via ingestion of the spores (for more information on spore
formation, go to General Characteristics). These spores can survive
up to two years on inanimate objects and are spread via the fecal-oral
route. The fecal-oral route most often involves someone touching a surface
contaminated C. difficile spores and then
touching their mouth with the contaminated hand. (Not surprisingly,
HANDWASHING is the best way to prevent C. difficile infections.) After ingestion, spores travel unharmed through
the acidic environment of the stomach and germinate into the vegetative
form.
vegetative
form.
From: (Public Domain) Centers for Disease Control and Prevention. 2009.
<URL:http://phil.cdc.gov/phil/home.asp>. Accessed 31 March 2009
Why does Clostridium difficile cause
disease in some people and not in others?
In an otherwise healthy person, the person’s
normal microflora of the intestines prevents C. difficile from
growing due to limited space and resources. However, when people are taking
significant amounts of antibiotics to treat another illness, the antibiotics
kill off the normal microflora of the intestines allowing C. difficile
to colonize the intestine and grow out of control. C. difficile is
most often acquired nosocomially (acquired secondary to a primary
hospitalization) because, in the hospital, patients are often on
broad-spectrum antibiotic therapy (antibiotics, such as clindamycin, used to
treat a number of bacterial infections) to prevent any infection.
Nevertheless, these antibiotics can cause pathogenic strains of C.
difficile to grow out of control. Pathogenic strains of C. difficile
can cause C. difficile- associated disease or CDAD.
CDAD affects more than 300,000 hospitalized patients yearly in the United
States.
How does Clostridium difficile cause
disease?
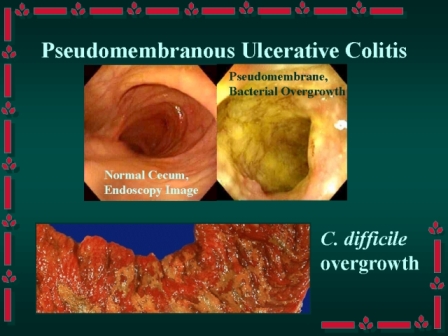
If the normal microflora of a person infected
with C. difficile has
been disrupted by antibiotic therapy, C.
difficile bacteria are able to reproduce in the intestinal crypts.
Pathogenic strains of C. difficile causes disease by the release of
two protein enterotoxins, toxin A and toxin B, which cause severe
inflammation and mucosal injury to the colon--colitis. At this point, the
toxins attract white blood cells to the area, and the white blood cells may
provide a protective immune response. However, if the white blood cells do
not provide the desired immune response, mild CDAD occurs. Nevertheless, the
toxins can actually kill the lining of the intestine, causing it to fall off
and mix with the white blood cells and give the appearance of yellow plaques
(patches) in the intestines. This is called pseudomembranous colitis because
the patches look like membranes but aren’t true membranes. (Check out
this video of a colonoscopy of a colon with pseudomembranous
colitis and note the yellow patches in the intestines.)
From: Johnson, M. T. 2009. Medical Microbiology
What are the symptoms of mild CDAD and severe
pseudomembranous colitis?
Mild CDAD * Non-bloody, watery diarrhea (5-10 watery stools
a day) * Low-grade fever *Abdominal cramping *Dehydration *Nausea *Loss of appetite
Pseudomembranous colitis (in
addition to mild symptoms) *Profuse watery diarrhea (greater than 10 watery
stools a day) *High fever (102°F—104°F) *Blood in the stool *Weight loss *Severe abdominal pain and tenderness *Death (6%-30% mortality rate) For information on treatments for CDAD and
pseudomembranous colitis, check out the
treatment page.
Who is most likely to get a Clostridium
difficile infection?
People who: *are taking more than one kind of antibiotic * have prolonged hospitalizations *are elderly *already have a disease of the intestine *are undergoing chemotherapy *have other serious diseases
Pathogenesis of Clostridium difficile-Associated Disease
Now that you have learned how C. difficile causes disease, you
should learn how the disease is
diagnosed, treated, and
prevented.
<URL:
http://web.indstate.edu/thcme/micro/anaercult/sld022.htm>.
Accessed 7 April 2009.
<URL:http://www.southend.nhs.uk/Hospital+Services/Other+Services/Infection+Control/Clostridium+Difficile/>.
Accessed 7 April 2007.