Interactions With Other Species
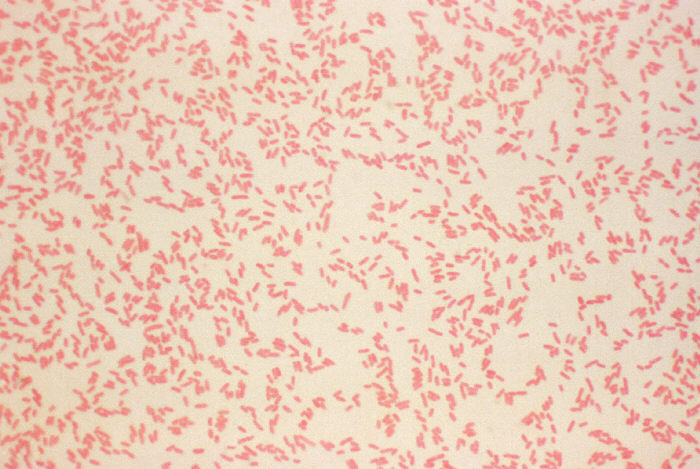
Yersinia enterocolitica isn’t the bacteria you want to run into on your late night walk home.
Just look at how scary it is!
Image courtesy of cdc.gov
It exhibits a parasitic relationship with its hosts. Many other bacterial species live in the same habitat as Yersinia enterocolitica but most, however, are mutualistic as compared to parasitic in the hosts gut. Yersinia enterocolitica is typically transmitted via the fecal oral route. People living in countries such a Germany where raw pork is commonly consumed have a higher incidence rate of the disease (Rosner, et al 2011).
Image courtesy of the Author
Even more so, young children are also prone to infection. In addition arthritis as a secondary immunologically mediated sequelae is most common among Scandinavians (Huovinen, et al 2010). The virulent strains of Y. enterocolitica cause the human disease Yersiniosis, which is most commonly characterized by heavy bouts of diarrhea. Y. enterocolitica infection is also associated with symptoms such as fever, diarrhea, nausea, vomit, and abdominal pain. The diseases caused include self-limiting gastroenteritis, fatal septicemia (Guinet, et al 2011), and further extra-intestinal complications caused by virulent Y. enterocolitica, such as liver and spleen abscesses, pneumonia, (to learn more about pneumonia click here!) septic arthritis, meningitis, empyema, and endocarditis. (Zheng, et al 2008) In most cases yersiniosis resolves without the need for treatment but in certain more severe cases antibitoic treatment is recommended. (To learn more about yersiniosis click here!) However Yersinia enterocolitica is generally resistant to penicillin and strains have been reported to be resistant to tetracycline, chloramphenicol, streptomycin, and kanamycin. The best course of antibiotics for Y. enterocolitca includes ceftriaxone, ceftazidime, cefotaxime, imipenem , aztreonam, and moxalactam.
Learn about toxin